Measuring brain tissue damage can identify cognitive decline
Rokna: By analyzing brain tissue damage using a new MRI evaluation tool, researchers accurately identified people with early signs of cognitive decline up to 70% of the time, a study published by the journal Academic Radiology found.
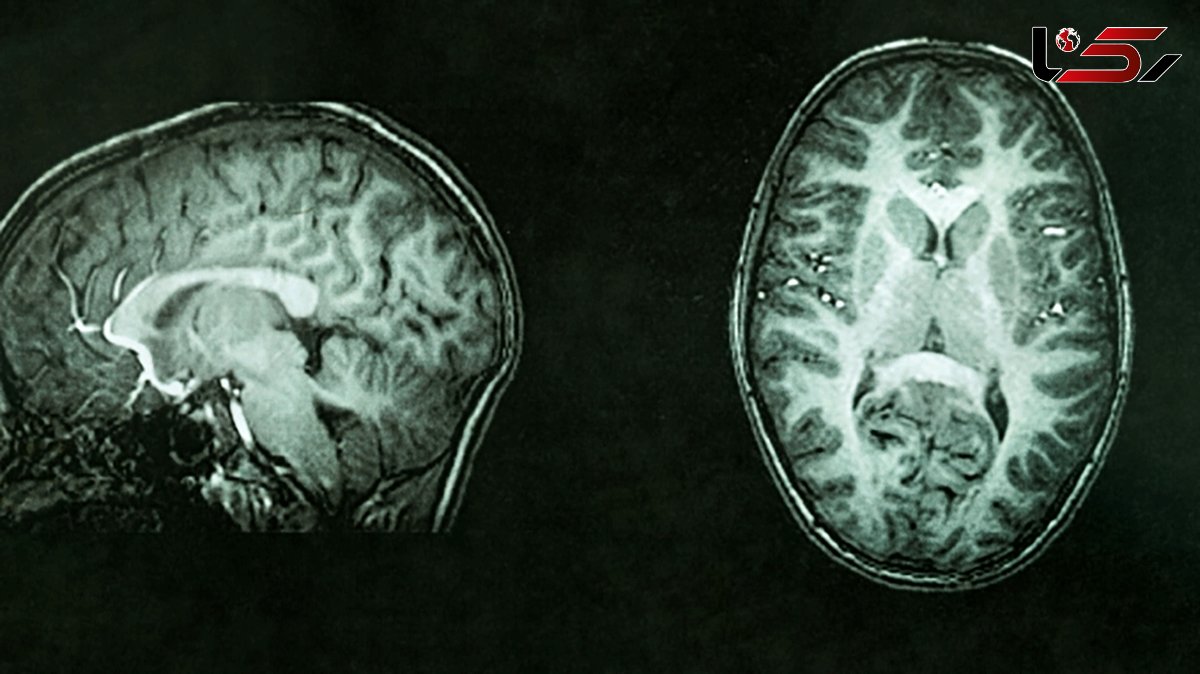
The approach uses magnetic resonance imaging to identify — and measure the number and size — of bright spots on the mostly gray images of the brain called white matter hyperintensities, or lesions, the researchers said, UPI reported.
These spots have long been linked to memory loss and emotional problems, especially as people age. Now, newly available MRI technologies could make it possible for them to be used for diagnosis of dementia, the researchers said.
"White matter lesion captured by MRI scans may reveal cognitive decline much earlier than behavioral symptoms," study coauthor Jingyun "Josh" Chen told UPI.
"Amounts of white matter lesions above the normal range should serve as an early warning sign for patients and physicians," said Chen, a research assistant professor of neurology at New York University Langone Health.
Roughly six million adults in the United States have dementia, according to the Alzheimer's Association.
Although the condition is common, it remains challenging to accurately diagnose, and no effective treatments exist, according to Chen and his colleagues.
The bright spots seen on MRI scans represent fluid-filled holes in the brain — lesions that are believed to develop from the breakdown of blood vessels that nourish nerve cells.
Earlier research has shown that increased numbers of spots and their presence in the center of the brain is linked with worsening dementia and other brain-damaging conditions, such as stroke and depression.
Current methods for grading white matter lesions, however, rely on little more than the "trained eye" using an imprecise three-point scale, according to the researchers.
The new tool, called the white matter hyperintensities toolbox and developed by Chen and his colleagues at NYU Grossman School of Medicine, is intended to provide neurologists with a uniform, objective method for calculating the spots' volume and location in the brain.
For this study, Chen and his colleagues randomly selected 72 MRI scans from a national database of adults age 70 and older in the US who participated in the Alzheimer's Disease Neuroimaging Initiative, a research project seeking to identify clinical, imaging, genetic and biochemical biomarkers for the early detection and tracking of Alzheimer's disease.
Using MRI techniques to map the brain's surface, the researchers then used the new tool to calculate the precise position and volume measurements for all observed white matter spots or lesions.
When researchers cross-checked their measurements, they found that seven out of 10 calculations correctly matched the patient's actual diagnosis.
With the standardized tracking and measuring tool, physicians could monitor the growth of white matter lesions in patients with suspected dementia, the researchers said.
White matter brain measures alone are not sufficient to diagnose early dementia, Chen said, but should be considered along with other factors. This includes a history of brain injury, memory loss and hypertension, as well as clear symptoms of cognitive decline or other brain and blood vessel diseases.
The researchers said they plan to broaden and test their measuring tool on 1,495 more brain scans to include a more diverse group of patients in the hope that it "may lead to the discovery of early biomarkers of dementia risks for individual patients."

Send Comments